ANKYLOSING SPONDYLITIS
What is ankylosing spondylitis?
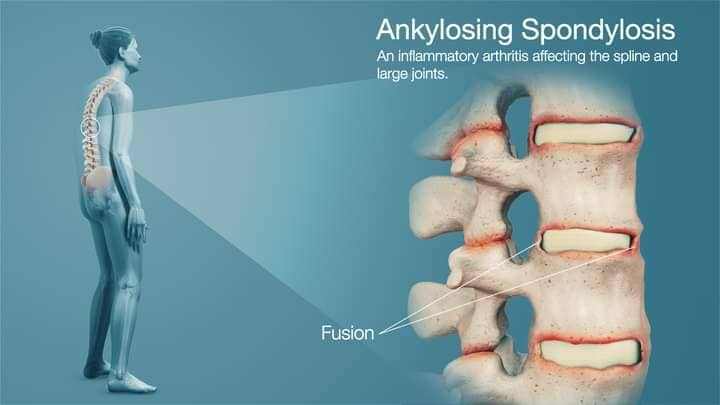
Ankylosing spondylitis (AS) (ank-ee-lo-zing spon-dee-li-tus) is a type of arthritis that mainly affects the back, by causing inflammation in the spine. This can make your back, rib cage and neck stiff and painful.
It often starts in people who are in their late teens or 20s.
In response to the inflammation, the body produces extra calcium around the bones of the spine. This can make extra bits of bone grow and cause your back and neck to be more stiff.
In rare cases some of the bones of the spine may link up, or fuse together because of the extra calcium. In serious cases this can make the spine curve forward more. You can reduce the risk of this happening, if you:
- keep active
- have effective medical treatment
- try to maintain a good posture.
While it mainly affects the neck and back, it can also cause pain and stiffness elsewhere in the body, including in the hips, shoulders and feet.
We don’t yet know what causes ankylosing spondylitis. To some extent it’s related to your genes, but the condition isn’t passed directly from a parent to their children. You can’t catch it from anyone else.
Conditions related to ankylosing spondylitis
Ankylosing spondylitis is a type of spondyloarthritis (spon-dee-lo-arth-rye-tus). This is the name for a group of conditions with similar symptoms – mainly pain and stiffness around the spine.
Here are some other types of spondyloarthritis:
- Non-radiographic (non-radio-graff-ick) axial spondyloarthritis – the main symptoms are similar to ankylosing spondylitis – pain and stiffness around the spine. But there won’t be physical changes to the back that can be seen on an x-ray. Some people with this condition are later diagnosed with ankylosing spondylitis.
- Psoriatic (sorry-at-ick) spondyloarthritis is a form of psoriatic arthritis that can occur alongside the skin condition psoriasis. People with psoriasis can get red, scaly patches of skin.
- Spondyloarthritis associated with inflammatory bowel disease, which is also called enteropathic (en-tur-o-path-ick) arthritis. This is related to bowel conditions such as Crohn’s disease or ulcerative colitis. The bowel is part of the digestive system that helps to break down the food we eat.
- Reactive arthritis is diagnosed when your arthritis is a reaction to an infection.
- Enthesitis (en-thur-si-tus)-related juvenile idiopathic arthritis is the name used when children and teenagers develop inflammation in entheses, the sites where tendons and ligaments attach to bones.
The rest of this content refers to ankylosing spondylitis. However, the treatment and self-management advice is very similar for people with other types of spondyloarthritis.
Symptoms
In the early stages, ankylosing spondylitis is likely to cause::
- stiffness and pain in your lower back in the early morning that lasts at least 30 minutes and then eases through the day or with activity
- pain that wakes you in the night
- pain in one or both buttocks and sometimes the backs of the thighs.
The condition can sometimes be mistaken for common backache.
Common backache often comes in short and painful spells. But the pain from ankylosing spondylitis is likely to be long lasting.
You may also have neck, shoulder, hip or thigh pain, which is worse when you’ve not been active for a time, for example if you sit for long periods working at a desk. Some people have pain, stiffness and swelling in their knees or ankles.
The pain and stiffness can vary over time. If most of the spine is affected, it can cause difficulty with activities that involve bending, twisting or turning.
Other possible symptoms include:
- soreness at the heel or in the arch of your foot
- pain and swelling in a finger or toe
- tenderness at the base of your pelvis, which can make sitting on a hard chair uncomfortable
- chest pain or a tightness around the chest that comes on gradually. This can make it difficult to take deep breaths. Your ribs may feel very tender, and you may find that you’re short of breath after even gentle activity. Coughing or sneezing may cause discomfort or pain.
- inflammation of the bowel. People with ankylosing spondylitis can develop bowel problems known as inflammatory bowel disease (IBD) or colitis. It’s a good idea to see your doctor if you have diarrhoea for more than two weeks or have bloody or slimy poos.
- fatigue, which is severe tiredness that doesn’t improve with sleep or rest. This can be caused by the condition itself, as well as by anaemia. This is when people have a lack of red blood cells, which carry oxygen around the body.
- depression and anxiety.
- inflammation of the eye, called either uveitis or iritis. The first signs are usually a painful and sometimes red eye. It may become uncomfortable to look at bright lights.
If one or both of your eyes are painful or red, or if you have changes to your vision such as partial loss of sight, blurred vision, floaters or sensitivity to light, it’s very important to get medical help as soon as possible. The best place to go is an eye casualty department. Your optician will be able to tell you where the nearest one is. You could also go to a GP surgery or an accident and emergency department. Treatment is usually with steroid eye drops, which are generally very effective.
Complications
If you’ve had ankylosing spondylitis for a long time or if the bones in your back have fused together, you may be at risk of bones in your back fracturing. A fractured bone in your spine can cause nerve damage.
It’s very important that a doctor treating you following a fall or an accident knows that you have ankylosing spondylitis.
If you have new unexplained pain in your spine or new weakness, numbness or tingling in your arms or legs, it’s very important to tell a doctor.
Some people with ankylosing spondylitis develop osteoporosis, a condition that causes bones to thin and be more likely to fracture.
If you have ankylosing spondylitis, or any kind of spondyloarthritis, it can make you slightly more at risk of problems such as a heart attack or a stroke. Taking drugs to reduce inflammation, as well as eating a healthy diet, not smoking and exercising regularly will reduce this risk.
Rarely, the top of your lungs may become scarred if your chest is affected by ankylosing spondylitis.
Although these problems can happen in people with ankylosing spondylitis, they are rare.
Diagnosis
Symptoms of ankylosing spondylitis can be similar to more common back problems, especially in the early stages.
Because of this, many people put up with the pain for some time before seeking help. It’s important to see a doctor as soon as possible if you suspect you have ankylosing spondylitis.
It’s usually diagnosed by a rheumatologist, these are doctors who specialise in conditions affecting the joints, bones and muscles.
There is no one test that can show for certain that you have ankylosing spondylitis. A diagnosis will be made based on several things, including:
- the history of your condition and the symptoms you’ve experienced, including whether pain and discomfort is waking you up during the second half of the night
- a physical examination
- blood tests, which may show inflammation
- x-rays or a magnetic resonance imaging (MRI) scan
- your age. It can be diagnosed at any age, but most often begins before the age of 40, and often much younger.
There are disease activity and pain scores that can help doctors diagnose ankylosing spondylitis. Your doctor will ask if you have key symptoms, such as swollen and painful joints, especially around the spine, and fatigue. You’ll be asked if you have pain in the mornings and how long for. Your answer to these questions could help lead to a diagnosis.
Blood tests can confirm whether you have the HLA-B27 gene. Most people with ankylosing spondylitis test positive for HLA-B27, but so do many people who don’t have the condition. A positive test may point to someone having ankylosing spondylitis, but it won’t confirm the diagnosis.
Treatment
A number of treatments can slow it down and treat pain and stiffness. Exercise and close attention to your posture are just as important to keep your spine mobile and help you to live a normal life.
Some of the drugs below can only be prescribed by a rheumatology consultant.
Physical therapies
Physiotherapy is a very important part of the treatment for ankylosing spondylitis. A physiotherapist can put together a programme of exercises to improve your muscle strength and help you maintain mobility in your spine and other joints.
It’s especially important to exercise your back and neck to avoid them stiffening into a bent position.
A physiotherapist will advise you on how to maintain good posture and may be able to offer you hydrotherapy, also known as aquatic therapy. This involves specific exercises for the spine, hips and shoulders carried out in a special warm-water pool.
Many people with ankylosing spondylitis find this therapy helpful and continue their programme at their local swimming pool or with their local National Ankylosing Spondylitis Society (NASS) group.
Spinal manipulation is not helpful or safe for people with ankylosing spondylitis as it could result in permanent damage to your spine or spinal cord. Manipulation is a type of manual therapy used to adjust parts of the body, joints and muscles to treat stiffness and deformity. It’s sometimes used in physiotherapy, chiropractic, osteopathy and orthopaedics.